Considerations for Reduced Usage of Quaternary Ammonium Compounds in Food Production and Healthcare Environments
Quaternary Ammonium Compounds (QACs or quats) are cationic, broad-spectrum antimicrobials that are widely used in food production and healthcare environments. Their low odor profile, ability to be used on soft metals, foaming capability and residual efficacy has made quats a biocide of choice for a variety of applications in these industries. However, the increase in resistance of microorganisms to QACs and the potential link between biocide resistance and antibiotic resistance has created the need to reevaluate the usage of these compounds in some sanitizer and disinfection treatments.
At low concentrations, QACs work by creating ‘holes’ in the cell membrane that cause the cell contents to leak out. At higher concentrations, they also target the carboxylic groups of the microbe and cause general coagulation within the cell.1 There are several well-characterized efflux pumps in adapted microbes that can make low concentrations of quats ineffective by simply pumping them out of the cell. Additionally, some gram-negative microorganisms have demonstrated an adaptive response to environmental stress that results in changes in the cell wall composition causing impermeability, which prevents the penetration of QACs into the cells.1 Of particular concern is the use of subinhibitory levels of QACs which may induce these adaptive responses in microbes.
“Microorganisms are the prime example of ‘survival of the fittest’, having continuously evolved to thrive in their ever-changing environments for billions of years. Because of this, scientists are constantly on the lookout for pathogens that may emerge and/or adapt in ways that make it difficult for currently available technologies to control them and render them particularly harmful to human health” said Crystal Maira, Principal at SciTech Consulting LLC. Some recent examples include Clostridium difficile, Candida auris and Listeria monocytogenes.
- C. difficile and C. auris are two emerging pathogens that have become a fundamental concern in the healthcare industry. Infection with either organism is extremely difficult to get rid of and patients with compromised immune systems are at the highest risk for contracting a hospital-acquired infection (HAI). It has been reported that “some medical facilities have had to replace floor and ceiling tiles to remove all traces of the organisms from patient rooms.”2 C. difficile is a spore-forming bacterium for which the spores have a very high resistance to conventional biocides. Exposure of C. diff planktonic cells to quats may stress the organism which facilitates formation of the spore state. Candida auris is a fungus that has recently emerged as a very serious threat in healthcare settings. In a 2017 commentary on the fungus C. auris given by Dr. Tom Chiller of the CDC, he stated: “This hardy yeast can live on surfaces for a month or more, and preliminary testing suggests that quaternary ammonium compounds commonly used for healthcare disinfection may not be sufficiently effective against C. auris.”3 While quats are effective general hospital disinfectants, the CDC recommends that EPA-registered products with claims against C. difficile be utilized in areas where C. auris is present until there are hospital disinfectant products registered with a specific C. auris claim.4
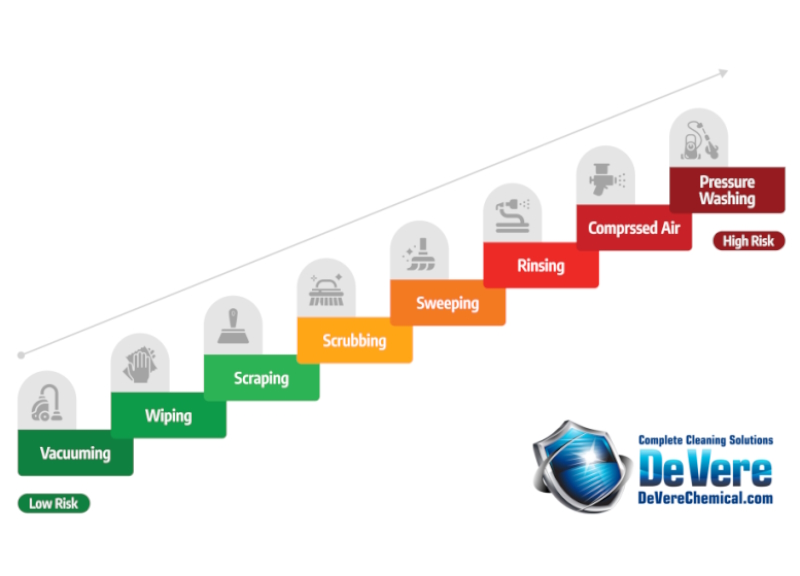
Listeria monocytogenes is a zero-tolerance organism that is a frequent problem encountered in food processing facilities. It is often found in environmental niches, floors, walls and drains and QACs are typically used to sanitize these surfaces. However, as Martinez-Suárez, et al. reported, dilution in the environment with water and organic matter results in QAC concentration gradients and “in certain cases, the relationship between low-level resistance and the environmental persistence of L. monocytogenes in different food production chains has been previously established.”5 Furthermore, investigations of listeriosis outbreaks usually trace the contamination source back to the processing environment and equipment. Thus, it is believed that the persistence of certain strains of L. monocytogenes even after cleaning and sanitizing is related to different situations that result in subinhibitory sanitizer concentrations and in turn adaption of the organism to the sanitizer(s) through genetic changes.5 The growing number of cases demonstrating a low-level resistance of QACs and persistence of L. monocytogenes in the food processing environments, it is recommended that technologies other than quats be utilized to sanitize areas where further dilution with water is likely, such as floors and drains.
The possibility of cross-resistance exists when both a biocide and antibiotics induce cell death via the same pathway or target.6 As such, the proper use of sanitizers and disinfectants, including the pre-cleaning of surfaces and using the indicated concentration and contact time, is essential. Akile Ozkan stated, “If subinhibitory concentrations are used, it will exert a selective pressure on the microorganism leading to the activation of stress responses. The end result of this would be a change in gene expression which will lead to superbugs that are resistant to disinfectants, while being unresponsive to antibiotics.”7 With some changes to sanitizing and disinfection protocols in the food and healthcare industries, it is hoped that this situation can be avoided.
References:
- To, M.; Favrin, S.; Romanova, N.; Griffiths, M. Postadapational resistance to Benzalkonium chloride and subsequent physiochemical modifications of Listeria monocytogenes. Appl. Environ. Microbiol. 68: 5258-5264.
- net. Emerging Super Fungus: Beginning of An Epidemic? April 9, 2019. https://www.worldhealth.net/news/emerging-super-fungus-beginning-epidemic/ (accessed on June 3, 2019)
- CDC Commentary. The Unexpected and Troubling Rise of Candida auris. August 24, 2017. https://www.medscape.com/viewarticle/884470 (accessed on June 5, 2019)
- United States Environmental Protection Agency. New Guidance on Environmental Control of Candida auris with Antimicrobial Pesticides. February 17, 2017. https://www.epa.gov/pesticides/new-guidance-environmental-control-candida-auris-antimicrobial-pesticides (accessed on June 6, 2019)
- Marteinez-Suárez JV, Ortiz S, López-Alonzo V. (2016) Potential Impact of the Resistance to Quaternary Ammonium Disinfectants on the Persistence of Listeria monocytogenes in Food Processing Environments. Front. Microbiol. 7:638. Doi: 10.3389/fmicb.2016.00638.
- Chapman, J. Disinfectant resistance mechanisms, cross-resistance and co-resistance. Int. Biodeterior. Biodegradation. 51: 271-276.
- Ozkan, A. Disinfectants as a double-edged sword: Are disinfectants promoting antimicrobial resistance? Catalyst. 3: 18-25.
Note of Appreciation:
Thank you to Crystal Maira, Principal at SciTech Consulting LLC for her work in putting this article together. Her expertise and resolve to improve our industry made this possible.
If you have any questions about the article or any of our products, please contact us.


[…] the U.S. National Institute of Health has empirically associated with the use of quats (click here for more […]
[…] Improper use of QACs can lead to superbugs. Proper use can make them one of the most efficient tools available in our war against pathogens. Generally, QACs can be used to disinfect flat, hard surfaces where the product will not end up in a drain or on the floor. For example, they work well when sanitizing desks, tables, food processing surfaces, and windowsills (primarily for mold inhibition). […]